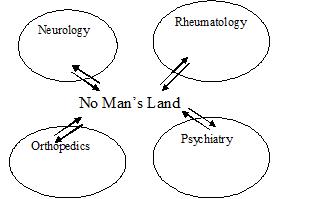
The majority of people with complex and unresolved pain find themselves vulnerable and frustrated in this “no-man’s land” of western medicine. Often a specialist will exclude a problem from his or her domain if it does not meet given criteria leading to a clear diagnosis. As such, he or she cannot treat the problem from his or her way of training and treatment. Even if a chronic pain problem is adequately diagnosed by a specialist, it is usually still very difficult to treat due to complex factors causing the problem not being addressed.
Often this is the case with the prescription of pain medications, where the pain may be reduced, but the origin problem is not understood or resolved. Drug treatments often result in significant side effects or other costs in function. Muscle relaxants, pain and sleeping medications, and now antidepressants are even part of chronic pain management. Drugs may work at first, but they often don’t fully resolve the problem. Even when they do lessen the pain, the side effects can be substantial; new problems such as drowsiness or cognitive impairment, and a client’s reduced ability to perceive feedback from the body to prevent injury, become weighed against the cost of tolerating pain.
We believe this arena becomes a professional “no-man’s land” in the modern medical system, where people go from one specialist to another, seeking an answer and definitive diagnosis, and ultimately, a final solution to the pain. It describes not the inadequacy of our system necessarily, but rather, the immense complexity of the problem. Any one medical specialty, such as neurology, rheumatology, psychiatry, or orthopedics, may not fully understand or treat persistent and complex pain on its own.
But not mysteriously, pain is a normal and adaptive response to any major problem where the body is telling us something is wrong. This is so, not just for the superficial injuries one gets of the skin, or the sprains and strains we get to muscles and tendons, and the degeneration of joints in arthritis. It also applies of course to internal disorders. Everybody knows about the general aches and pains and muscle tightness when you get the flu. This is usually a normal response to any major pathology where the body is telling us something is wrong.
In the case of an acute flu virus invasion the response is quick and very noticeable. But often imbalances of health happen slowly and have complex origins – these can be difficult to link to a single specific internal problem. In this way, chronic pain is often a generalized reaction to accumulation of stressors, be it physical/metabolic exhaustion, environmental toxins, dietary deficiencies, persistent insomnia, chronic emotional stress, etc. More often, these stressors are presented in combination and interact with each other. Eventually, the issue is not just a pain message from the body, but turns into a chronic musculoskeletal dysfunction too. In the beginning these messages are adaptive, and represent a internal warning can create reflex protective postures. For example, a problem in the lungs pneumonia is sometimes perceived as painful and tight pectoral muscles. Here a person has his shoulders hunched forward to lesson the pain. This posture may be protective for an acute injury of the lung, but for chronic issues is not helpful. Here, over time tight chest muscles may restrict chest mobility and the vital capacity of the lung.
In the next blog we will explore the possible mechanisms that explain how we can perceive internal problems externally. These signals can be valid early detection systems that allow us to be in better tune with our health.




